Newsletter
The College of Reproductive Biology (CRB) is a not-for-profit special interest group of the American Association of Bioanalysts (AAB).
The Pursuit of the Perfect Consent
Melanie Clemmer, Ph.D., HCLD(ABB)
Publication Committee
Recently my clinic has been focusing on updating our consents for all parts of the IVF process and the topic of making better consents has been central in my mind, thus it became the focus of this article. Since consents are such an integral part of determining what we can and cannot do legally in the laboratory, I thought that this would be a good opportunity to remind everyone of good practices to keep in mind when developing and utilizing consent documentation. I am certainly not a legal expert, so for something as engrained in legal quagmire as the disposition of gametes and embryos please consult with appropriate legal counsel. If it’s been more than a few years since your practice has taken an in depth review of the consents used in your practice then there are likely improvements that can be made to the consenting process, starting with the documents used. Prevention is better than reaction when it comes to legal matters and here are ten items to keep in mind when reviewing and updating consents for your practice.
1. Know the local, state and national laws that impact disposition options. As we recognize one year since the overturning of Roe v. Wade by the Supreme Court, this is more important than ever. In specific states, some disposition options for embryos changed overnight. Stay on top of the changing legal landscape in your state to provide your patients with appropriate disposition options. Be familiar with the differences in ownership for autologous and donor gametes and/or embryos as these determine which parties can authorize consent.
2. Consult available resources. Consult appropriate legal counsel in the development of your consent documents to ensure they are complete, worded appropriately and follow local, state and national laws. The legal team can assist you in determining the level of detail that needs to go into building a good consent. There are great examples of consents available for SART members on SART.com. These example consents were developed by both laboratory and legal experts in the field and can be customized or at least serve as a template for your own documents.
3. Give well-defined instructions to patients. Use simple language that can be understood by most, even those patients with lower health literacy. The top of our disposition consents used to state ‘Please complete the entire document and return to the clinic.’ While this seems clear, probably about one-quarter of our disposition consents get returned back to the patient for correction; usually because the document was not notarized. We have updated our wording to state, ‘Please complete the entire document. This document MUST BE notarized before being returned to the clinic.’ We will see if this small, but more direct wording change improves our rate of consents that are returned to us and correctly filled out on the first try. In the pursuit of building a better consent, we still have not found a fool-proof method to prevent patients from selecting more than one option when presented with multiple options. There will always be the one that selects each option despite the clear instruction of ‘select ONLY ONE of the following options.’
4. List clear timeframes. Use reasonable time frames for responses and do not put in time frames that contradict each other. For instance, on one of our old consents we stated that patients have thirty (30) days to pay their annual storage bill for frozen specimens or we could discard their specimen(s) and in the same document state that patients must go five (5) years without payments or contact with the clinic before we would discard their specimens once they had been declared abandoned. Many times, just having a clear time frame can lay out a discrete plan with expectations from both parties.
5. Take time to explain consents before they are signed. This can be done in person or via electronic consenting services but the importance of taking time to walk patients through the options presented to them and the statements they are expected to understand cannot be overemphasized.
6. Be thorough. Determine ahead of time what specific consents are needed at your clinic. For instance, if you have information on the ICSI or assisted hatching (AH) process embedded in each consent then a separate consent document just for ICSI and AH is not needed. Having one larger consent for each procedure rather than one small one for each step has been working better for us. It allows the patients to follow what will happen from start to finish in one document rather than signing multiple documents. Yes, some consents are lengthy and should be kept separate (like those for genetic testing). Make the consents lay out the plans of the patient for the cycle; for instance, how many embryos to thaw, what gender embryos to thaw, whether or not PGT is being done and for how many embryos.
7. Review and update consents regularly. If there are amounts for payment embedded into your consent or agreement documentation then keep it up to date. If your annual charge for cryopreserved specimens goes up and the consent signed by the patient states a lower value then there will be more questions from patients that must be addressed. Keep terminology up to date. If your consent documents use PGD instead of PGT then an update to the language in your consents is overdue. Regular review of consents is good laboratory practice and part of the accreditation requirements.
8. Learn from your past experiences. Think of those scenarios that arose in the past that could not be completely addressed by simply looking at the consent. For us it was the death of a patient that had clearly indicated to give their specimens to their partner upon death. In contact with the surviving partner, they desired to take ownership of the specimens but have not returned updated documentation after months. For that patient we wait (for now), but in our updated consents, we have now included a time frame in which documentation must be completed before specimens would be discarded.
9. Look over all consent documents for completeness after they are returned to the clinic in a timely manner. Have a dedicated individual or team of individuals that review consents for completeness when they are returned. There can be no elections left unchosen or signatures not signed. Even more critical is to make certain the patient(s) marked only one option when choices are to be made. There should be no ambiguity in the elections of the patient(s) once the document is completed. When preparing for a patient cycle the day before oocyte retrieval or embryo transfer is not the time to determine there are issues with the consents.
10. Build a complete consenting process that works. Have a few individuals that participate in and oversee the consent process from start to finish and require that they do it well with attention to detail. Make review of consents by laboratory staff second nature in the planning steps. There should be no ambiguity when it comes to what the laboratory (and clinic) is legally allowed to do based on the patient(s) consent. Diligently work through the entire consenting process to see where errors are being made (either by patients or clinic/laboratory staff) and strive to do better using a quality improvement approach.
There are no perfect consents as new technology comes about, legal requirements get altered, patient relationships become complex and there is a stream of “well, this never happened before’s’’ that will arise right after you update your consents. The goal of a quality consent document should be to clearly present the primary points of general expectations, risks, options and obligations and that once signed, clearly details to clinic and laboratory staff the wishes of the patient(s) and their understanding of the procedures they are giving consent to. There should be clarity for the staff when the consent process is started with the development of a good consent document and carried through with attention to detail.
Earn ABB/PEER Continuing Education Credit ⇒CRB News Articles
08/11/2023
Vol 12, No. 1
08/11/2023
From the CRB President
08/11/2023
CRB Symposium Returning To JW Marriott Las Vegas May 7-10, 2024
08/11/2023
Upcoming 2024 AAB Meeting in Las Vegas
08/11/2023
The Pursuit of the Perfect Consent
08/11/2023
Earn ABB/PEER Continuing Education Credit Attending Postgraduate Courses at ASRM 2023
08/11/2023
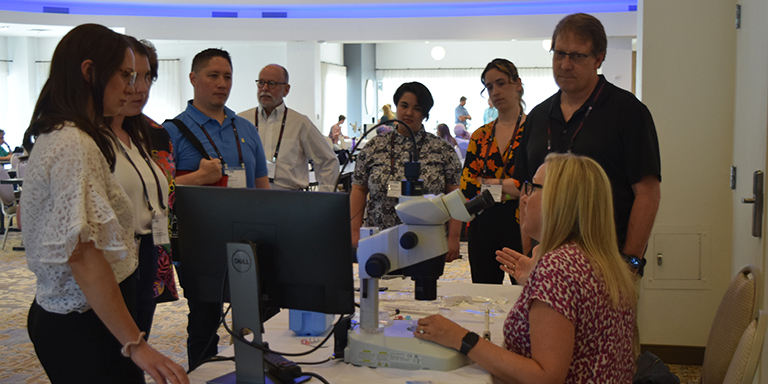
25th CRB Symposium and 65th AAB Educational Conference Scrapbook
08/11/2023
Thank you to the sponsors of AAB/CRB 2023
08/11/2023
ALS/ELS Certifications for Andrologists and Embryologists
CRB Standing Rules - Log in to view