‒

Newsletter
The College of Reproductive Biology (CRB) is a not-for-profit special interest group of the American Association of Bioanalysts (AAB).

Revolutionizing IVF Success: The Role of AI in Enhancing Key Performance Indicators
Murat Basar, Ph.D., M.Sc.
A quality management system is vital for effectively managing an in vitro fertilization (IVF) clinic's laboratory. It comprises quality control, quality assurance, and quality improvement activities. Performance indicators referred to as key performance indicators (KPIs), are required for monitoring and continual improvement. This section assesses technical KPIs in the embryology lab and clinical KPIs.
Key Performance Indicators in IVF Laboratories
The Vienna Consensus concluded that 12 KPIs might be considered integral to a QMS since they encompass the most essential steps within the IVF laboratory process.
ICSI and IVF Fertilization Rate
The ICSI fertilization rate is widely reported and effectively indicates gamete quality and operator competency. The ICSI 2PN rate is affected by the numerous criteria utilized to perform ICSI, which might be an oversight of the indicator. Even though the definitions can differ within the literature, according to a report of an expert meeting on the development of art laboratory performance indicators by the ESHRE Guideline Group, the ICSI Normal Fertilization Rate KPI is defined as the number of fertilized oocytes on Day 1 (presence of 2PN and 2PB assessed at 17 ± 1 h post-injection) as a function of all MII oocytes injected. This consensus also suggests that regarding ICSI fertilization rates, it may be necessary to exclude cases where lower fertilization rates are expected, such as in vitro matured metaphase I oocytes, artificially activated oocytes, the use of testicular sperm, and cases of globozoospermia and asthenozoospermia. Similarly, another study published by Hammond et al. used ICSI fertilization KPI as suggested by the Vienna Consensus definition to assess if KPIs detect shifts in laboratory performance that precede changes in clinical outcomes. In addition, Zaca et al. validated the Vienna consensus to monitor the outcome of treatments involving women of different age ranges in 2022 and concluded that ICSI fertilization rates were comparable between the Vienna consensus and the older female age groups (72.3% and 75.3%, respectively, p=NS). In a very recent consensus between the Italian Society of Fertility and Sterility and Reproductive Medicine (SIFES-MR) and the Italian Society of Embryology, Reproduction, and Research (SIERR), in addition to acceptance of the definition and importance of this KPI, they also suggested that the frequency of analysis should be monthly or every 100 cycles, whichever comes first. Similarly, the Normal IVF Fertilization Rate KPI is defined as the number of fertilized oocytes on Day 1 (presence of 2PN and 2PB assessed at 17 ± 1 h post-insemination) as a function of all COCs inseminated in Vienna Consensus. Vaiarelli et al. formulated this KPI as the number of oocytes with 2PN and 2 PB / number of cumulus-oocyte complexes. They suggested tracking the KPI monthly or every 100 cycles, whichever occurs first. Like the ICSI fertilization rate, when Zaca et al. compared the Vienna consensus parameters in advanced-age females, the comparison of standard IVF fertilization rates did not show significant differences (67.2% and 67.3%, respectively, p=NS).
IVF Polyspermy Rate
Three or more pronuclei indicate aberrant fertilization, caused by polyspermy or nondisjunction, defined as failure to extrude the second PB. In a study published by Sun et al. in 2023, it was reported that there appears to be a slight increase in the risk of polyspermy when the number of oocytes is more than 15. Oocyte immaturity, oocyte over-maturity, and/or an exceptionally high concentration of motile spermatozoa in the insemination volume can all lead to polyspermy. When the literature was reviewed regarding KPI studies in ART, it was seen that polyspermy was not included much other than the Vienna consensus. According to the consensus, the calculation of polyspermy PI was suggested as the proportion of inseminated oocytes with more than two pronuclei on Day 1 (17 ± 1 h post-insemination) and is needed to provide the information to interpret any observed variations in the standard fertilization rate.
1 PN Rate and Polyploidy Rate
Most professionals agree that embryos with only one pronucleus (1PN) are aberrant and should not be used in therapeutic settings. Therefore, it is standard procedure to reject these embryos after a fertilization check. When we assessed the studies published by Pirea et al., Variaelli et al., Zaca et al., Hammond et al., and Wang et al., we concluded that polyspermy rate was not considered an important KPI when compared to other evaluated PIs. Although many publications do not mention the number of PNs as a PI should be considered, as also mentioned in the Vienna Consensus, it can provide a marker of a problem in gamete handling or culture conditions and should be low under normal conditions. After insemination by IVF, which happens in 1-5% of instances, oocytes containing a single pronucleus may indicate parthenogenetic activation, asynchronous pronuclei appearance, or fertilization and syngamy. On the other hand, the reported diploidy rate of 1PN oocytes resulting from ICSI is only 7-14%, and the resulting embryos contain genetic abnormalities.
ICSI Damage Rate
Oocyte degeneration rate, or ICSI damage rate, is considered essential. Therefore, the number of oocytes injured during ICSI and/or seen during fertilization, over the number of injected oocytes, is the definition of the ICSI damage rate. We strongly agree that monitoring this indicator helps understand laboratory performance, oocyte quality, and operator competency. Additionally, the damage rate may be a sign of technical issues.
Total Fertilization Failure Rate
Insufficient motile sperm, inadequate sperm function, or poor oocyte activation can lead to poor or failed fertilization. The Vienna Consensus recommends individually examining each case of failure to achieve regular fertilization in an ICSI cycle.
Zaca et al. found no significant differences in fertilization and embryo cleavage KPIs between the Vienna consensus and older age groups. However, Campos et al. reviewed that 1-3% of ICSI cycles suffer from oocyte activation deficit (OAD), which affects fertilization and is a recognized cause of infertility. OAD occurs due to sperm or oocyte-related problems and has received less attention until recently.
The Proportion of Embryos with > Eight Cells on Day3
This KPI measures how well the culture system supports embryo development for transfers on days two or three. A recent study showed that embryos with more than eight cells on day three had a higher percentage of good-quality blastocysts. The KPI is calculated as the number of embryos with at least eight cells on day 3 divided by the number of normally fertilized oocytes, according to the Italian Society of Fertility and Sterility and Reproductive Medicine (SIFES-MR) and the Italian Society of Embryology, Reproduction and Research (SIERR) consensus.
Total Blastocyst Development Rate
The blastocyst is a subjective standard based on evaluating blastocyst morphology. The "Day 5 blastocyst development rate" is a KPI that only tracks blastocyst formation on Day 5. Assessing the impact of culture changes on developmental potential is challenging, as delayed blastocyst development is not always undesirable.
Blastocyst Utilization Rate
Even though most of the practices tend to use total blastocyst development rate as a KPI, blast utilization rate is an important parameter to be considered since it is defined as the number of embryos utilized (transferred or cryopreserved) per number of 2PN zygotes in the same cycle. This metric is frequently shown in research, but because it depends on cryopreservation and embryo transfer techniques as well as patient desire, it cannot determine competency and benchmark levels.
Oocyte & Embryo and Blastocyst Cryo-Survival Rate
Survival rates are considered essential KPIs indicating the embryology laboratory's success. The oocyte survival rate is the proportion of morphologically intact oocytes at ICSI following freezing and warming. The cleavage stage embryo survival rate is defined as the percentage of viable embryos that were thawed and had at least 50% of their blastomeres intact. Finally, the blastocyst cryo-survival rate is defined as at least 75% of cells intact after thawing-warming and agreed to be calculated as the number of survived blastocysts/numbers of thawed-warmed blastocysts.
AI Integration in IVF Laboratories
AI and machine learning technologies are employed in various aspects of the IVF process to enhance the efficiency and accuracy of IVF treatments.
Data Analysis: AI algorithms excel in processing and analyzing the vast datasets generated in IVF treatments. They can identify patterns and correlations that may not be evident to human observers, leading to more informed decision-making.
- Predictive Modeling: AI can predict outcomes based on historical data, such as the likelihood of fertilization, embryo development, and successful implantation. This predictive capability is invaluable in customizing treatment plans for individual patients.
- Embryo Selection: Researchers are developing image analysis tools that utilize AI to assess embryo quality more accurately. These tools analyze images of embryos to identify those with the highest potential for successful implantation, going beyond the capabilities of traditional morphology-based assessments.
- Laboratory Automation: AI is significantly enhancing laboratory automation in IVF. Automated systems, guided by AI algorithms, can handle repetitive tasks such as pipetting, sorting, and labeling with greater precision and consistency than manual methods. This automation reduces the risk of human error and increases the efficiency of the IVF process. Automated incubators, for example, can maintain optimal conditions for embryo culture, while robotic systems can assist in the delicate process of embryo selection and transfer.
- Real-time Monitoring for Quality Control: AI's role in real-time monitoring is a game-changer for quality control in IVF laboratories. Advanced AI algorithms, integrated with time-lapse imaging technology, continuously monitor the development of embryos. This monitoring provides invaluable data on the health and viability of embryos, crucial for making informed decisions about which embryos to transfer. By tracking development patterns and identifying any deviations or abnormalities early on, AI-enhanced real-time monitoring ensures a higher standard of quality control. This level of monitoring not only aids in selecting the best embryos for transfer but also contributes to a deeper understanding of embryonic development, leading to continuous improvement in IVF practices and protocols.
- Customized Treatment Protocols: By analyzing patient-specific data, AI can assist in developing personalized treatment protocols, potentially increasing the success rates of IVF procedures.
Challenges in Quality Control and KPI Measurement
IVF laboratories require assistance to maintain consistent quality control due to procedure variability and human error. The challenges of IVF treatments are compounded by the subjective nature of specific assessments, like embryo grading. Additionally, managing and analyzing the vast amount of data generated is complex and often overwhelming.
Ethical and Practical Considerations
The integration of AI in reproductive medicine raises ethical concerns, such as the implications of algorithmic decision-making and data privacy. Additionally, integrating AI into existing workflows and ensuring proper staff training are practical challenges that need addressing.
Future Directions and Conclusion
The use of AI in IVF labs shows promise for boosting success rates. This article discusses the potential benefits of AI in improving the quality control of IVF. AI could lead to a new era in assisted reproductive technology by emphasizing the importance of implantation rate as a primary indicator of overall IVF success. Integrating AI into IVF laboratories can revolutionize the field, offering more precise, efficient, and personalized treatments.
References:
- ESHRE Special Interest Group of Embryology and Alpha Scientists in Reproductive Medicine. “The Vienna consensus: report of an expert meeting on the development of ART laboratory performance indicators.” Reprod Biomed Online. 2017 Nov;35(5):494-510. doi: 10.1016/j.rbmo.2017.06.015. Epub 2017 Aug 4.
- Basar M, Unsal E, Ergun Y. Embryology with precision: effective quality control in the in vitro fertilization laboratory. Curr Opin Obstet Gynecol. 2024 Jun 1;36(3):200-207. doi: 10.1097/GCO.0000000000000945. Epub 2024 Apr 10. PMID: 38572581.
CRB News Articles
7/18/2024
Vol 13, No. 1
07/18/2024
Introduction from the CRB President
07/18/2024
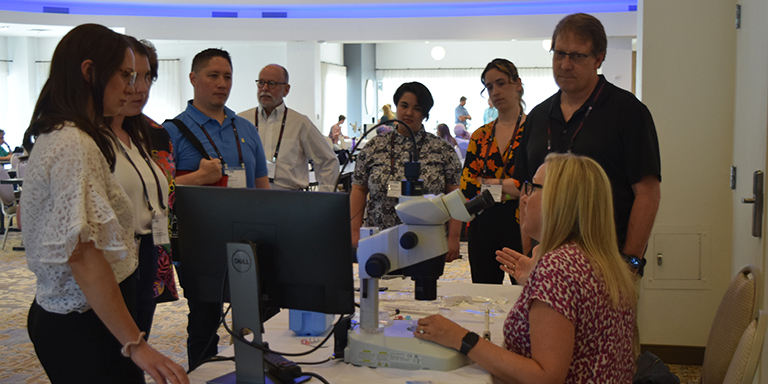
2024 CRB Symposium Recap
07/18/2024
Wishing Tammie Schalue a Happy, and Well-Deserved, Retirement
07/18/2024
Laboratory Management and Leadership Development Workshop
07/18/2024
Revolutionizing IVF Success: The Role of AI in Enhancing Key Performance Indicators
07/18/2024
CLIA Registration Fees are Increasing
07/18/2024
Recent CMS/CLIA Changes to Proficiency Testing Requirements
07/18/2024
FDA Imposes New Regulations on Laboratory Developed Tests
07/18/2024
2025 Symposium Dates & Location
07/18/2024
California Recognizes Clinical Reproductive Biologists with the Passage of Senate Bill 1267
07/18/2024
Earn ABB/PEER CE Credit by Attending ASRM!
07/18/2024
Andrology Antics by Samuel Prien, Ph.D., HCLD(ABB)
07/18/2024
A special thanks to the CRB Publication Committee members:
CRB Standing Rules - Log in to view